Imaging Case 9:
Papillary thyroid carcinoma
Papillary thyroid carcinoma is the most common type of thyroid cancer. Depending on the stage at diagnosis, it is treated with a combination of (total) thyroidectomy, cervical lymphadenectomy and/or radioiodine treatment. If a lymph node metastasis is detected at follow-up, resection of the invaded lymph nodes can be considered. However, confirming intraoperatively that the target lymph nodes have been resected can be a challenge.
In this clinical case we show how a detailed view of resected lymph nodes can be obtained with high-resolution specimen PET-CT imaging. This information can help the surgeon determine if the targeted lymph nodes have been resected right at the point of surgery. This case is presented with the support of dr. Valérie Vergucht and prof. dr. Bieke Lambert of AZ Maria Middelares, Ghent, Belgium.
Patient History
A 42 year-old woman was diagnosed with papillary thyroid carcinoma and underwent primary thyroid resection, cervical lymphadenectomy and radioiodine treatment. A second lymphadenectomy was indicated after recurrence of lymph node metastasis was suspected on whole-body 18F-FDG PET-CT.
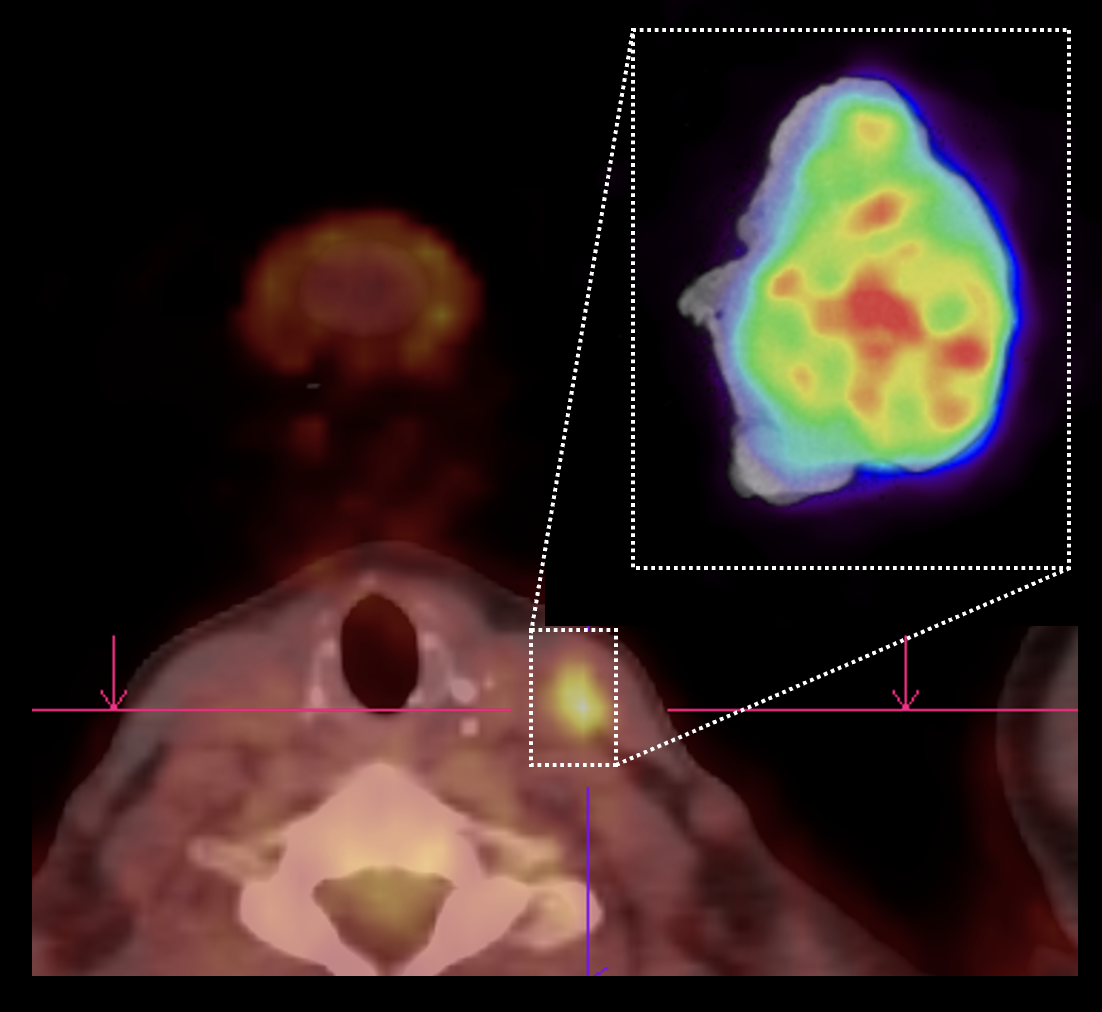
Follow-up whole-body 18F-FDG PET-CT imaging three months after the second lymphadenectomy demonstrated persistent small but PET-positive lymph nodes in region 4 and 3 left. Their metastatic invasion was confirmed by fine needle aspiration cytology. Hence, a third lymphadenectomy was scheduled with the aim of removing these two lymph nodes. The preoperative whole-body PET-CT images are shown in fig. 1. The SUVmax of both suspect lymph nodes was 4.97 (region 4) and 6.14 (region 3).
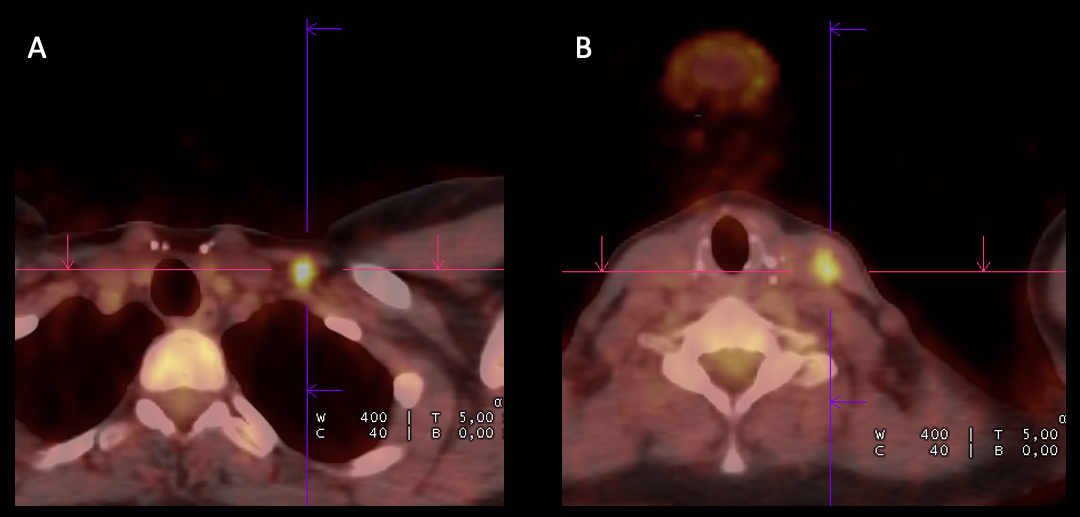 Figure 1: whole-body 18F-FDG PET-CT images of the two suspected lymph nodes in region 4 (A) and region 3 (B) left. The SUVmax of both lymph nodes was 4.97 and 6.14 respectively.
Figure 1: whole-body 18F-FDG PET-CT images of the two suspected lymph nodes in region 4 (A) and region 3 (B) left. The SUVmax of both lymph nodes was 4.97 and 6.14 respectively.
The surgical procedure was expected to be particularly difficult as the same region needed to be accessed for the third time. To provide as much information as possible about the resected tissue to the surgeon – and help ensure that the targeted lymph nodes are removed – intraoperative specimen PET-CT imaging was utilized.
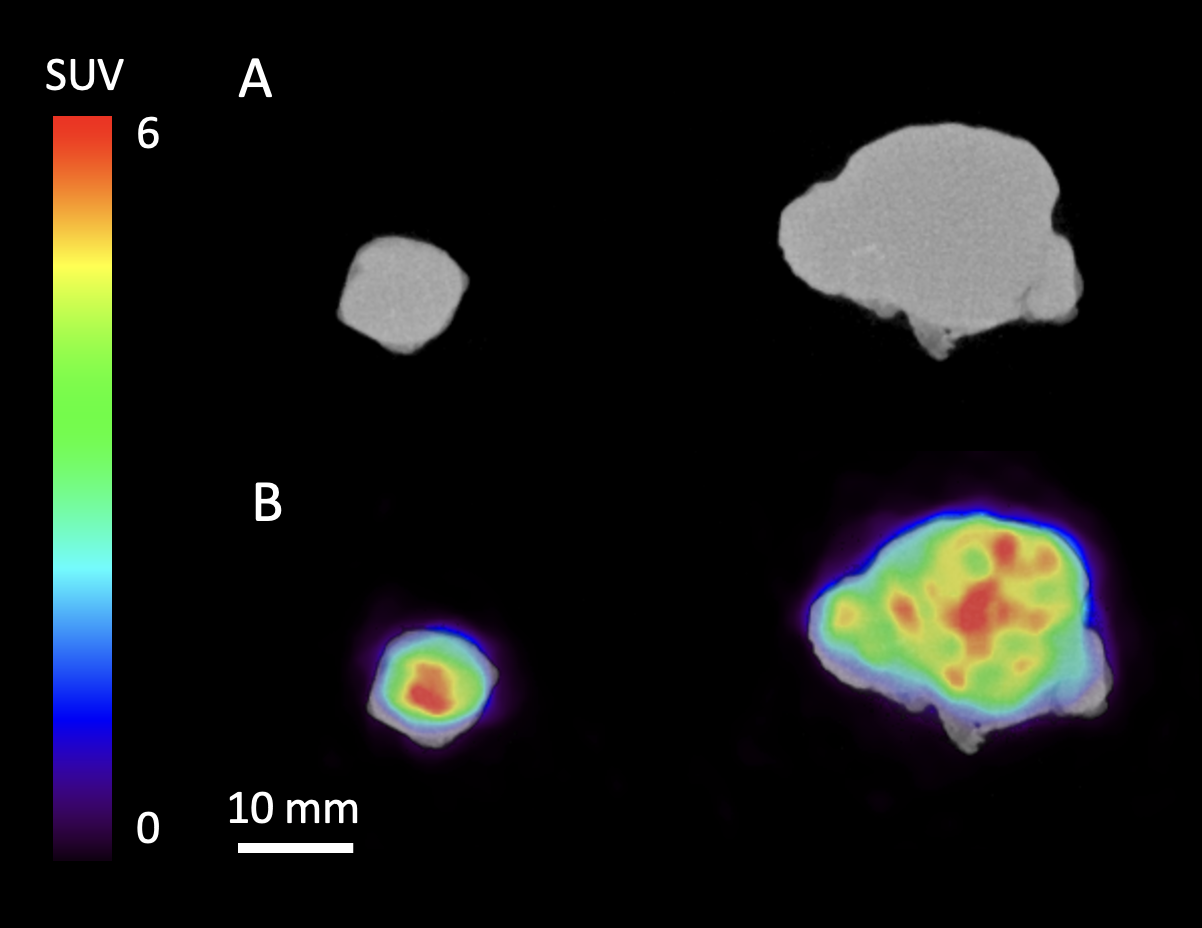 Figure 2: high-resolution specimen CT (A) and PET-CT (B) images of the resected lymph nodes. The node from region 4 is shown on the left, the node from region 3 is shown on the right.
Figure 2: high-resolution specimen CT (A) and PET-CT (B) images of the resected lymph nodes. The node from region 4 is shown on the left, the node from region 3 is shown on the right.
PET-CT specimen images
The patient was injected with 4 MBq/kg 18F-FDG at the nuclear medicine department approximately 1 hour before the start of surgery. Resection of the lymph nodes was completed at approximately 140 min after injection. Immediately after resection, a high-resolution specimen PET-CT image was acquired in the operating theatre. The images are shown in fig. 2.
The images of both lymph nodes clearly show increased 18F-FDG uptake with SUVmax of 7.3 (region 4) and 6.8 (region 3). Due to the high spatial resolution of the specimen PET-CT images, heterogeneity of the radiotracer uptake can be appreciated within the lymph nodes. These images were interpreted during surgery in the operating theatre to help confirm that the target lymph nodes were resected.
Histopathology
Histopathology confirmed quasi complete metastatic invasion of both resected lymph nodes by papillary thyroid carcinoma cells. The node from region 4 was 9 mm in the largest direction, the node from region 3 was 22 mm in the largest direction. On histopathology the surgical margins were free, with the closest margin at 0.1 mm for both lymph nodes.
Discussion and conclusion
This case illustrates how specimen PET-CT imaging can be used to visualize lymph nodes with suspected papillary thyroid carcinoma during surgery. This information, provided at the point of surgery, can help the surgeon ensure that the lesions targeted for resection are indeed removed. In this presented case, there was an excellent agreement with histopathology which is deemed the gold standard for final assessment of surgical success.
REFERENCES
Filetti, S. et al. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology, Volume 30, Issue 12, 1856 – 1883.